What is Rectal Prolapse?
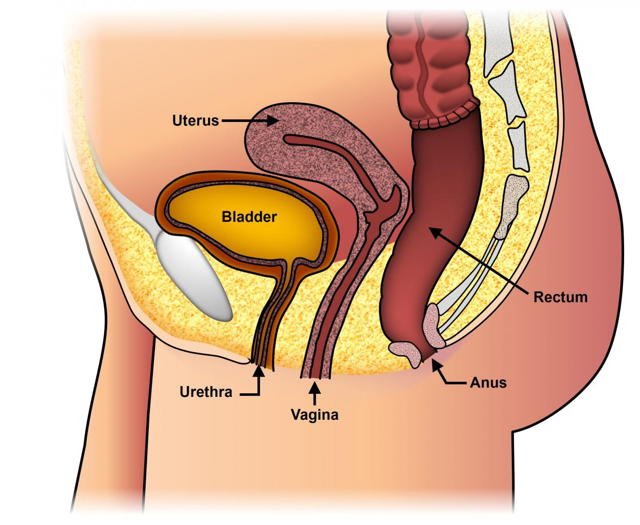
Rectal Prolapse is a condition in which the rectum (the last part of the large intestine before it exits the anus) loses its normal attachments inside the body, allowing it to telescope out through the anus, thereby turning it “inside out”. While this may be uncomfortable, it rarely results in an emergent medical problem. However, it can be quite embarrassing and often has a significant negative impact on patients’ quality of life.
Although the operation is not always needed, the definitive treatment of rectal prolapse requires surgery.
Presentation
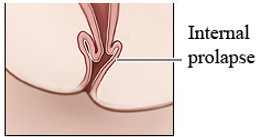
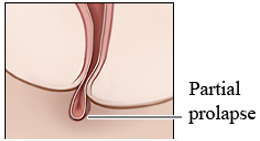
Rectal prolapse tends to present gradually. Initially, the prolapse comes down with a bowel movement (BM) and then returns to its normal position. Patients may later describe a mass or “something falling out” that they may have to push back in following a BM. Until the prolapsed rectum goes back in, patients may feel like they are “sitting on a ball”.


Rectal prolapse may be confused with significant hemorrhoid disease and can even be confusing at times to physicians not frequently evaluating and treating this problem.
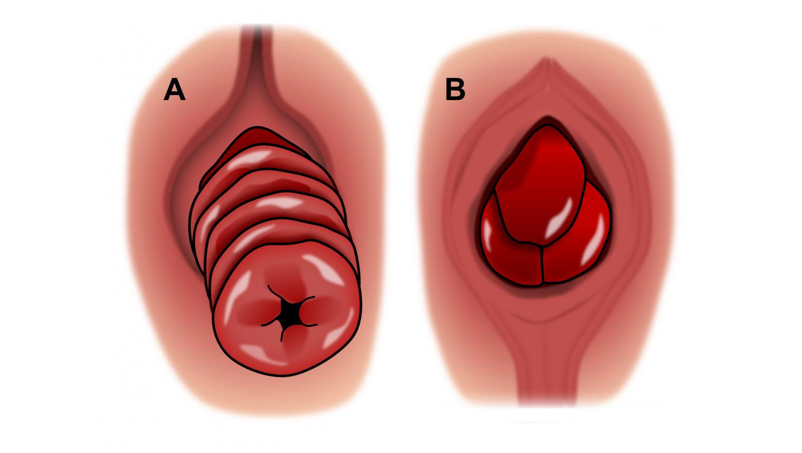
A = Rectal Prolapse B = Hemorrhoids
Over time, prolapsed rectal mucosa may become thickened and ulcerated causing significant bleeding. Rarely, the prolapse becomes stuck or “incarcerated” outside the anus – a situation that could require emergent surgery.
Surgery For Rectal Prolapse
There are two general approaches to surgery for rectal prolapse – abdominal operations (through the belly) and perineal operations (through “the bottom”). Both approaches aim to stop the prolapse from occurring again and usually result in a significant improvement in the quality of life.
The choice of surgery type depends on both patient factors and procedural factors. Patient factors include the patient’s age, sex, bowel function, continence, prior operations, and severity of associated medical problems. Procedural factors include the extent of prolapse, what effect the procedure might have on bowel function and incontinence, complication rates of the procedure, recurrence rates of the procedure and the individual surgeon’s experience.
After your treatment, the nurse will go over few instructions and you will be given a prescription for few medications and an appointment for a postoperative checkup few days later.

