What is Anal Abscess?
An anal abscess is an infected cavity filled with pus found near the anus or rectum. Ninety percent of abscesses are the result of an acute infection in the internal glands of the anus. Occasionally, bacteria, fecal material or foreign matter can clog an anal gland and tunnel into the tissue around the anus or rectum, where it may then collect in a cavity called an abscess.
CLASSIFICATION
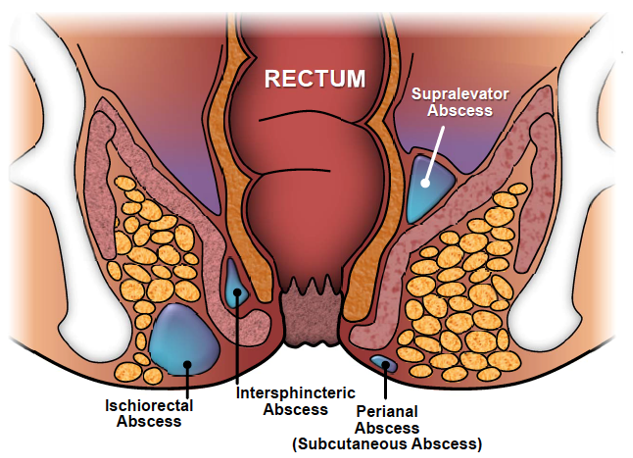
Anal abscesses are classified by their location in relation to the structures comprising and surrounding the anus and rectum: perianal, ischioanal, intersphincteric and supralevator. The perianal area is the most frequent and the supralevator the least. If any of these particular types of abscess spreads partially circumferentially around the anus or the rectum, it is termed a horseshoe abscess.
Symptoms of Anal Abscess
Anorectal pain, swelling, perianal cellulitis (redness of the skin) and fever are the most common symptoms of an abscess. Occasionally, rectal bleeding or urinary symptoms, such as trouble initiating a urinary stream or painful urination, may be present.
Examination of Anal Abscess
A careful history regarding anorectal symptoms and past medical history are necessary, followed by a physical examination. Common findings leading to the diagnosis of a perirectal abscess are fever, redness, swelling and tenderness to palpation. However, while most abscesses are visible on the outside of the skin around the anus, it is important to recognize that there may be no external manifestation of an abscess, other than a complaint of rectal pain. A digital rectal exam may cause exquisite pain.
Treatment of Anal Abscess
The treatment of an abscess is surgical drainage under most circumstances. An incision is made in the skin near the anus to drain the infection. This can be done in a doctor’s office with local anesthetic or in an operating room under deeper anesthesia. Hospitalization may be required for patients prone to more significant infections, such as diabetics or patients with decreased immunity.
Up to 50% of the time after an abscess has been drained, a tunnel (fistula) may persist, connecting the infected anal gland to the external skin. This typically will involve some type of drainage from the external opening. If the opening on the skin heals when a fistula is present, a recurrent abscess may develop. Until the fistula is eliminated, many patients will have recurring cycles of pain, swelling and drainage, with intervening periods of apparent healing.
Antibiotics alone are a poor alternative to drainage of the infection. The routine addition of antibiotics to surgical drainage does not improve healing time or reduce the potential for recurrences in uncomplicated abscesses. There are some conditions in which antibiotics are indicated, such as patients with compromised or altered immunity or in the setting of extensive cellulitis (spreading of infection in the skin).
After your treatment, the nurse will go over few instructions and you will be given a prescription for few medications and an appointment for a postoperative checkup few days later.

